Clubitis disease is a relatively rare and intriguing condition that has been the subject of increasing interest in the medical community. Characterized by an unusual inflammation of the distal phalanges, or the ends of the fingers and toes, clubitis disease can lead to the deformation commonly known as "clubbing." While many associate clubbing with chronic pulmonary conditions, clubitis disease can arise from various underlying health issues, making it a complex subject worthy of exploration. Understanding its etiology, symptoms, and treatment options is crucial for healthcare providers and patients alike.
In recent years, clubitis disease has garnered attention not only for its distinctive physical manifestations but also for its potential to signal serious systemic disorders. Clubbing, the primary symptom, results from changes in the soft tissue and bones beneath the nail beds, leading to an enlargement and rounding of the fingertips. This alteration can be quite alarming for those affected and often prompts further medical investigation to uncover the root cause. Such investigations are essential, as clubitis disease can be indicative of conditions ranging from heart and lung diseases to gastrointestinal disorders.
For those living with clubitis disease, the journey can be fraught with uncertainty. The complexity of the condition, coupled with the potential for underlying health issues, necessitates a comprehensive approach to diagnosis and treatment. By delving into the nuances of clubitis disease, we aim to provide a clearer picture of this enigmatic condition, offering insights into its symptoms, causes, and management strategies. Through increased awareness and understanding, individuals affected by clubitis disease can find reassurance and hope in the pursuit of effective care and improved quality of life.
Table of Contents
- What is Clubitis Disease?
- Symptoms of Clubitis Disease
- What Causes Clubitis Disease?
- How is Clubitis Disease Diagnosed?
- Treatment Options for Clubitis Disease
- Risk Factors Associated with Clubitis Disease
- Living with Clubitis Disease: What to Expect?
- Preventive Measures for Clubitis Disease
- How Clubitis Disease Impacts Daily Life?
- Latest Research on Clubitis Disease
- Is Clubitis Disease Common in Children?
- Psychosocial Aspects of Clubitis Disease
- Frequently Asked Questions
- Conclusion
What is Clubitis Disease?
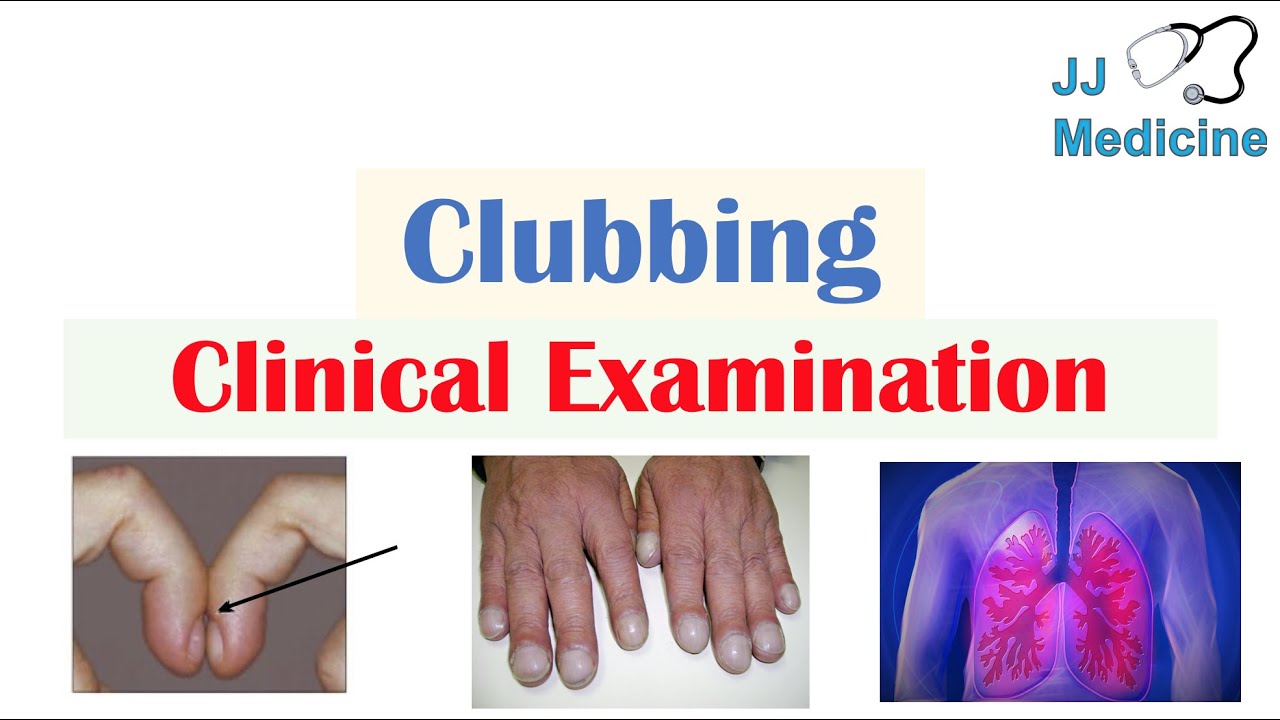
Clubitis disease is a medical condition characterized by the swelling and deformation of the soft tissues and bones at the ends of the fingers and toes, typically referred to as "clubbing." This condition, while often associated with chronic diseases such as pulmonary or cardiovascular disorders, can actually be indicative of a variety of systemic health issues. The term "clubitis" derives from the appearance of the affected digits, which become rounded and bulbous, resembling small clubs.
The pathophysiology behind clubitis disease involves changes in the vascularization of the distal phalanges, leading to increased blood flow and subsequent tissue proliferation. This process results in the characteristic enlargement and alteration of the nail beds and surrounding tissues. Although the condition itself is benign, its presence can be a crucial diagnostic clue pointing towards more serious underlying health concerns.
Understanding clubitis disease requires a multidisciplinary approach, combining insights from dermatology, rheumatology, and internal medicine. The condition is often a symptom rather than a standalone disease, necessitating comprehensive evaluation to determine its root cause. While the exact prevalence of clubitis disease is not well-documented, it remains a significant concern due to its association with potentially life-threatening illnesses.
Symptoms of Clubitis Disease
The primary symptom of clubitis disease is the visible change in the appearance of the fingers or toes, known as "clubbing." This symptom is usually the first indication that something may be amiss. Clubbing occurs in stages, starting with the softening of the nail beds, followed by the development of a convex curvature of the nail, and ultimately resulting in the enlargement of the fingertips.
Other symptoms that may accompany clubbing include:
- Nail changes: Nails may become shiny and appear to "float" on the nail bed.
- Swelling: The tissue beneath the nail bed becomes thickened, leading to a swollen appearance.
- Pain or tenderness: Some individuals may experience discomfort or sensitivity in the affected areas.
It is important to note that the presence of clubbing does not in itself cause pain or functional impairment. However, the underlying condition responsible for clubitis disease may lead to additional symptoms, depending on its nature. For example, if clubitis disease is associated with a lung condition, respiratory symptoms such as cough or shortness of breath may also be present.
What Causes Clubitis Disease?
The etiology of clubitis disease is complex and multifactorial, often involving a combination of genetic, environmental, and systemic factors. While the exact mechanisms remain unclear, several potential causes have been identified:
Underlying Health Conditions
Clubitis disease is frequently associated with chronic illnesses, particularly those affecting the pulmonary and cardiovascular systems. Some common conditions linked to clubbing include:
- Lung diseases: Chronic obstructive pulmonary disease (COPD), cystic fibrosis, and lung cancer are known to cause clubbing.
- Heart conditions: Congenital heart defects and endocarditis can lead to clubitis disease.
- Gastrointestinal disorders: Conditions like Crohn's disease and ulcerative colitis have been implicated in clubbing.
Genetic Factors
There is evidence to suggest that genetics may play a role in the development of clubitis disease. Family history of clubbing or related conditions can increase an individual's risk of developing the condition.
Environmental Factors
Exposure to certain environmental factors, such as smoking or occupational hazards, may contribute to the onset of clubitis disease, particularly when combined with other risk factors.
Understanding the underlying causes of clubitis disease is crucial for effective management and treatment. By identifying and addressing the root cause, healthcare providers can offer targeted interventions to alleviate symptoms and improve patient outcomes.
How is Clubitis Disease Diagnosed?
Diagnosing clubitis disease involves a thorough clinical evaluation and a comprehensive medical history. The process typically includes several steps to ascertain the presence of clubbing and its underlying cause:
Physical Examination
During a physical examination, a healthcare provider will assess the appearance of the fingers or toes, looking for signs of clubbing. The evaluation may include measuring the angle between the nail and the cuticle and checking for swelling of the soft tissue around the nails.
Medical History
A detailed medical history is essential to identify any potential underlying conditions. The healthcare provider may inquire about symptoms related to respiratory, cardiovascular, or gastrointestinal health, as well as any family history of similar conditions.
Diagnostic Tests
Depending on the suspected underlying cause, additional diagnostic tests may be recommended:
- Blood tests: To check for markers of inflammation or infection.
- Imaging studies: Chest X-rays or CT scans to evaluate lung and heart health.
- Pulmonary function tests: To assess lung function.
Accurate diagnosis of clubitis disease is crucial for determining the appropriate treatment and management strategies. By identifying the root cause, healthcare providers can tailor interventions to address both the symptoms and the underlying condition.
Treatment Options for Clubitis Disease
Treatment for clubitis disease primarily focuses on addressing the underlying condition responsible for the clubbing. Since clubitis is often a symptom rather than a standalone condition, effective management requires a targeted approach:
Medical Interventions
Depending on the underlying cause, treatment options may include:
- Medications: Anti-inflammatory drugs, antibiotics, or other medications to manage the underlying condition.
- Surgery: In some cases, surgical intervention may be necessary to correct structural abnormalities or remove tumors.
- Lifestyle changes: Smoking cessation, dietary modifications, and regular exercise to improve overall health and reduce symptoms.
Supportive Care
Supportive care plays a crucial role in managing the symptoms of clubitis disease and improving the quality of life for affected individuals. This may include:
- Physical therapy: To maintain mobility and function in the affected areas.
- Psychological support: Counseling or support groups to address the emotional and psychological impact of the condition.
While there is no specific cure for clubitis disease, addressing the underlying cause can often lead to significant improvement in symptoms and overall well-being. A multidisciplinary approach, involving collaboration between healthcare providers, patients, and their families, is essential for optimal management.
Risk Factors Associated with Clubitis Disease
Several risk factors have been identified that may increase an individual's likelihood of developing clubitis disease. Understanding these factors can help in early detection and intervention:
Chronic Health Conditions
Individuals with chronic health issues, particularly those affecting the lungs, heart, or gastrointestinal system, are at increased risk for developing clubitis disease. Conditions such as COPD, cystic fibrosis, and congenital heart defects are commonly associated with clubbing.
Genetic Predisposition
A family history of clubbing or related conditions can suggest a genetic predisposition to clubitis disease. Genetic factors may influence an individual's susceptibility to developing the condition, particularly in the presence of other risk factors.
Lifestyle and Environmental Factors
Lifestyle choices, such as smoking, can contribute to the development of clubitis disease. Occupational exposure to certain environmental hazards may also play a role in increasing the risk of clubbing.
Recognizing these risk factors is crucial for early detection and intervention. By addressing modifiable risk factors and monitoring individuals with known predispositions, healthcare providers can implement preventive measures to reduce the incidence and impact of clubitis disease.
Living with Clubitis Disease: What to Expect?
Living with clubitis disease can present unique challenges, but with proper management and support, individuals can lead fulfilling lives. Understanding what to expect and how to cope with the condition is essential for maintaining a positive outlook:
Coping with Symptoms
The visible changes in the appearance of the fingers or toes can be distressing for some individuals. Coping strategies may include:
- Seeking support: Joining support groups or speaking with a counselor to address emotional and psychological concerns.
- Practicing self-care: Engaging in regular exercise, maintaining a balanced diet, and prioritizing mental health.
Managing Underlying Conditions
Effective management of the underlying condition responsible for clubitis disease is crucial for reducing symptoms and improving quality of life. This may involve regular medical check-ups, adherence to treatment plans, and open communication with healthcare providers.
By taking an active role in their health and well-being, individuals with clubitis disease can navigate the challenges of the condition and maintain a high quality of life. With the support of healthcare providers, family, and friends, they can find ways to thrive despite the presence of clubitis disease.
Preventive Measures for Clubitis Disease
While it may not be possible to prevent clubitis disease entirely, certain measures can reduce the risk of developing the condition or mitigate its impact:
Addressing Modifiable Risk Factors
Making lifestyle changes can significantly reduce the risk of clubitis disease, particularly for those with known risk factors:
- Quit smoking: Smoking cessation is one of the most effective ways to reduce the risk of clubbing, especially in individuals with underlying lung conditions.
- Maintain a healthy lifestyle: Regular exercise, a balanced diet, and stress management can improve overall health and reduce the likelihood of developing chronic conditions associated with clubitis disease.
Regular Medical Check-ups
For individuals with known risk factors or a family history of clubitis disease, regular medical check-ups are essential for early detection and intervention. Monitoring health and addressing any emerging symptoms promptly can help manage the condition effectively.
By taking proactive steps to address risk factors and prioritize health, individuals can reduce their risk of developing clubitis disease and improve their overall well-being. Preventive measures, combined with ongoing medical care, can make a significant difference in managing the condition.
How Clubitis Disease Impacts Daily Life?
Clubitis disease can have a profound impact on an individual's daily life, affecting both physical and emotional well-being. Understanding these impacts is crucial for developing effective coping strategies:
Physical Limitations
The physical changes associated with clubitis disease, such as the enlargement of the fingertips, can lead to challenges in performing daily tasks. Fine motor skills may be affected, making activities like writing, typing, or buttoning clothes more difficult.
Emotional and Psychological Effects
The visible nature of clubbing can lead to self-consciousness and social anxiety for some individuals. The condition may also bring about feelings of frustration or helplessness, particularly if it is associated with a chronic underlying illness.
Despite these challenges, individuals with clubitis disease can find ways to adapt and thrive. By seeking support, adopting coping strategies, and staying engaged in their health management, they can improve their quality of life and maintain a sense of normalcy.
Latest Research on Clubitis Disease
Ongoing research into clubitis disease continues to shed light on its causes, mechanisms, and potential treatments. Recent studies have focused on several key areas:
Genetic and Molecular Insights
Advancements in genetic research have highlighted potential molecular pathways involved in the development of clubitis disease. Understanding these pathways may lead to targeted therapies and improved diagnostic techniques.
Novel Treatment Approaches
Research into novel treatment options, including pharmacological interventions and lifestyle modifications, holds promise for improving symptom management and patient outcomes. Studies exploring the role of anti-inflammatory medications and dietary supplements are particularly noteworthy.
As research progresses, it is hoped that new insights will lead to more effective management strategies for clubitis disease. By staying informed about the latest developments, healthcare providers and patients can make informed decisions about treatment and care.
Is Clubitis Disease Common in Children?
Clubitis disease is relatively uncommon in children, but it can occur in association with certain congenital conditions or chronic illnesses. When clubbing is observed in a pediatric patient, it often warrants further investigation to identify any underlying health concerns.
Common Causes in Children
In children, clubitis disease is typically linked to congenital heart defects or cystic fibrosis. These conditions can lead to changes in blood flow and oxygenation, resulting in the characteristic clubbing of the fingers and toes.
Diagnosis and Management
Diagnosing clubitis disease in children involves a comprehensive evaluation, including a physical examination and medical history. Additional diagnostic tests may be necessary to identify the underlying cause. Management strategies focus on addressing the root condition and providing supportive care to improve the child's quality of life.
While clubitis disease is less common in children, early detection and intervention are crucial for preventing complications and optimizing outcomes. By working closely with pediatric healthcare providers, families can ensure that their child receives the best possible care.
Psychosocial Aspects of Clubitis Disease
The psychosocial aspects of clubitis disease are an important consideration for both patients and healthcare providers. The condition can affect an individual's emotional and social well-being, making it essential to address these concerns as part of a comprehensive management plan:
Emotional Impact
The visible nature of clubbing can lead to self-esteem issues and social anxiety. Individuals may feel self-conscious about their appearance, leading to avoidance of social situations and a decrease in overall quality of life.
Support and Resources
Access to psychological support, such as counseling or support groups, can be invaluable for individuals coping with the emotional challenges of clubitis disease. Connecting with others who have similar experiences can provide a sense of community and understanding.
By addressing the psychosocial aspects of clubitis disease, individuals can improve their emotional well-being and build resilience in the face of challenges. A holistic approach to care, encompassing both physical and emotional health, is essential for optimal outcomes.
Frequently Asked Questions
- What is the primary symptom of clubitis disease?
The primary symptom of clubitis disease is the visible change in the appearance of the fingers or toes, known as "clubbing."
- Can clubitis disease be cured?
There is no specific cure for clubitis disease, but addressing the underlying cause can often lead to significant improvement in symptoms.
- Is clubitis disease hereditary?
While there is evidence to suggest a genetic component, clubitis disease is often associated with underlying health conditions rather than being directly inherited.
- Can lifestyle changes help manage clubitis disease?
Yes, lifestyle changes such as smoking cessation, regular exercise, and a balanced diet can improve overall health and help manage symptoms.
- Are children affected by clubitis disease?
Clubitis disease is relatively uncommon in children but can occur in association with certain congenital or chronic conditions.
- How is clubitis disease diagnosed?
Diagnosis involves a physical examination, medical history, and potentially additional diagnostic tests to identify the underlying cause.
Conclusion
Clubitis disease, with its distinctive manifestation of clubbing, represents a fascinating intersection of dermatology, rheumatology, and internal medicine. While the condition itself is benign, its presence can signal serious underlying health issues, necessitating a thorough and multidisciplinary approach to diagnosis and treatment. By understanding the causes, symptoms, and management strategies for clubitis disease, healthcare providers and patients can work together to address both the visible manifestations and the root causes of this complex condition.
With ongoing research and a focus on holistic care, there is hope for improved outcomes and quality of life for those affected by clubitis disease. Through increased awareness, proactive management, and supportive care, individuals can navigate the challenges of the condition and lead fulfilling lives. The journey with clubitis disease may be challenging, but with the right resources and support, it is one that can be undertaken with confidence and optimism.
You Might Also Like
Meet Sally Bakula: A Trailblazer In Her FieldDevon Larratt: Champion Arm Wrestler And His Family Life
All About Benjamin Netanyahu's Daughter: Family, Career, And More
Insights Into The World Of Drake Dick: A Comprehensive Analysis
Insights Into Samantha Hegseth's Role On Outnumbered
Article Recommendations
- Craig Jones Bjj Record A Deep Dive Into The Acclaimed Brazilian Jiujitsu Black Belts Achievements
- Devin Haney Wife All You Need To Know About His Life Partner And Relationship
- Exploring The Life And Partner Of Joe Cole Insights Into The Actors Journey